In their book “Super-bugs, the arms race against bacteria”, William Hall and colleagues highlight that an estimated 1.5 million deaths a year are attributable to drug resistant bugs caused by antimicrobial resistance (AMR). They describe AMR as “a truly global problem that has the potential to affect every person on the planet”. Indeed, a great deal of that potential is already being realised, with an estimated 1.5 million deaths a year already attributable to drug resistant bugs. If this is a global issue, it makes sense for teams across the world to work together to solve these global issues. In this blogpost, we want to highlight some of the great work that is happening across the globe, but also ask: “What Next?”.
The solution to the problem of AMR is not just to produce new and better drugs – that takes time, and a great deal of money. We must also reduce our use of antibiotics when they are not needed. Sadly, it seems that they are used unnecessarily twenty percent of the time in the UK* and Australia is above the their peers in the OECD when it comes to prescription volumes. Getting people – both patients and physicians – to change their behaviour in this domain has been the subject of study by behavioural scientists, including our own work with Public Health England, which found a national decline in prescribing from sending a letter from the chief medical officer utilising social norms to the top 20% of prescribers in their area, and, in the United States.
This week, the Behavioural Economics Research Team in the Australian Department of Health (BERT) and the Behavioural Economics Team of the Australian Government (BETA), published their own study, testing five different messages to physicians, replicating and expanding upon previous work, the most effective of which reduced antibiotic prescribing by an impressive 12%.
Building on the evidence in this area, they tested some novel ways of highlighting that GPs were prescribing more than their peers. This included a simple graph which showed how many pills GPs were prescribing in relation to their peers. This turned out to be the most effective of their interventions. They were also able to provide individual-level data on GPs’ prescribing information. This is not available in the UK, where it is only available at the practice level; but it makes for a powerful and personal message. It turns a global problem into one that they and they alone can do something about.
This is a great example of BI units around the world building on each others’ work to push the frontiers of BI.
Combining Data Science and Behavioural Insights
So, what can the Behavioural Insights community do next to tackle AMR?
If we’re to successfully combat this threat to our future as a species, we’re going to need to bring every tool at our disposal to bear on it. As readers of this blog know, BIT London and Sydney have been experimenting with the use of data science techniques to improve public policy outcomes. For the rest of this post, we consider the two points of confluence between behavioural and data science in fighting drug resistance. The first point looks at how we can take a targeted preventative approach to stop GPs becoming high prescribers and the second highlights how we can become better at targeting those who already are high prescribers.
Targeting GPs at risk
The majority of behavioural science interventions against AMR have targeted prescribers who are already among the worst offenders – in our case, the top 20% of prescribers in a local area, and in the BERT and BETA study it was the top 30%. By the time these interventions are brought to bear, years of unnecessary prescriptions have been written and filled.
This issue is analogous to the dilemma that a GP faces. They do not know whether or not someone with a sore throat cold might go on to develop pneumonia or just have a sore throat.
Our job is slightly easier than the GPs’, as we have access to more systematic data. We zoomed into practices who were not previously high prescribers, but then escalated their use to become high prescribers. We used a machine learning technique to work out whether these practices had something else in common.
Making use of publicly available data from the UK, which included prescribing data and reviews of GP practices left by patients, we were able to identify 40% of these escalating prescribers about twice as efficiently as chance.
This is early work, and we could certainly do better with more data, but this model gives a basis for pre-emptively offering support for doctors at risk of over-prescribing before they do so.
As mentioned above, the only data we used was publicly available data, which in the UK is at the practice level. It could be the case that some of the variation is accounted for by GPs moving practices. By having access to individual level data, we could provide more support to GPs to stop them prescribing inappropriately.
Targeting Interventions
The second point of confluence is in our ability to target behavioural interventions to doctors who are most likely to respond to the intervention. This would avoid sending an intervention to people who are going to get no benefit, or who will even respond by increasing their prescribing.
To do this, we used a form of analysis developed by Susan Athey and Guido Imbens from Stanford University called Causal Trees, which allows us to identify, within our randomised controlled trial, which groups of GPs experienced positive, no, or negative effects from the letters we sent.
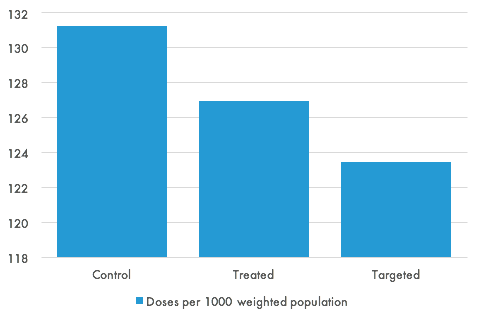
The graph below shows the estimated effect of this targeting. The graph shows the trial results for the treatment and control groups, and the estimated level of prescribing if all practices had been assigned to the intervention which the algorithm predicted would have the largest effect. Even in a simple, two-arm trial, we can gain almost as much from targeting as the treatment itself.
What’s next?
Behavioural Insights units around the world are coming together and building on each others’ work to deal will the global issue of AMR. Tackling the biggest problems that we face globally is going to take more than either behavioural science or machine learning can offer – but if we bring them together, their impacts could be greater than the sum of their parts.
* We as the authors debated at length as to whether we should emphasise the fact that 80% of the prescriptions are being used in necessary cases.