The British Medical Association’s NHS backlog data analysis (December 2022 data) shows that around 7.2 million people in England are waiting for treatment, and the number waiting over a year is about 240 times greater than before COVID-19. Reducing NHS waiting lists is a key political priority, and one of the Prime Minister’s five pledges in his January 2023 speech.
NHS England set out its plan for tackling the elective care backlog (excluding primary and community care, urgent and emergency care, and mental health services) in February 2022. Its goal is to progressively eliminate long waits, tackling waits of over 18 months by April 2023 (current estimates suggest up to 220,000 patients could have been waiting this long by April), over 65 weeks by March 2024, and over 52 weeks by March 2025.
What can trusts and healthcare providers do now and within their existing resources to reduce the backlog?
NHS England reports it will work towards these goals by increasing health service capacity, prioritising diagnosis and treatment, transforming the way elective care is provided, and providing better information and support to patients. NHS England’s ability to realise its plans will be crucial to tackling the backlog.
There is a great deal of work under way to address the issue, with many innovative solutions being tested. Many of the plans are ambitious, require substantial funding and may take some time to put in place. In the interim, what can NHS trusts and healthcare providers do now and within their existing resources to reduce the backlog?
There is increasing recognition that behavioural factors are key to improving health in the long-term: around 40% of years of life lost in England are the result of behavioural and lifestyle factors (eg tobacco and diet). But it may be less obvious that behavioural science could help with the elective backlog.
Surely we just need more doctors, beds, testing facilities, and so on? Yet behavioural science can sometimes help by ‘oiling the works’, or removing key frictions, so that existing staff and systems can work better.
Over the next five days we’ll present a number of ideas, studies and evidence on the role behavioural insights can play in reducing healthcare backlog.
Interventions informed by behavioural science are particularly suited to the resource-constrained NHS environment as they often only involve tweaks to existing systems, making them cheaper and faster to implement than other interventions.
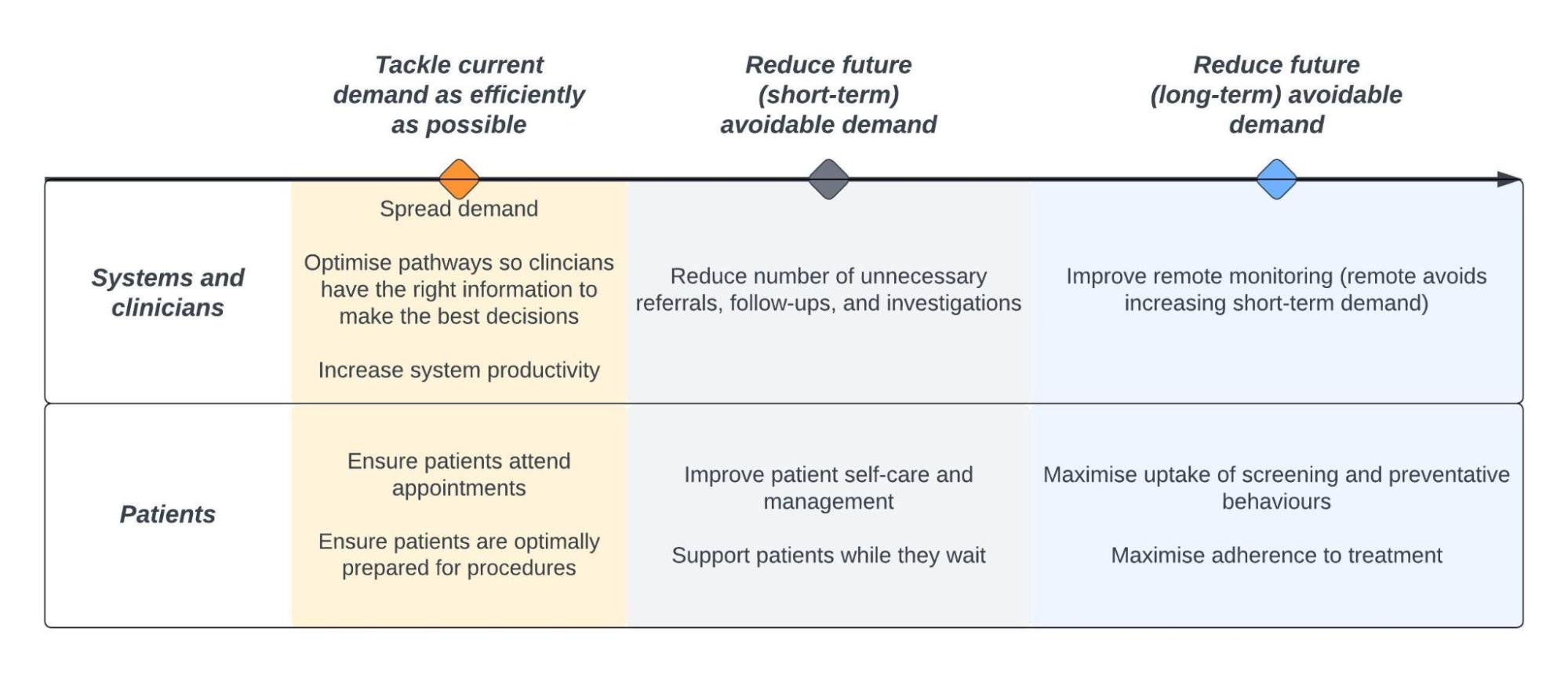
Past behavioural interventions have delivered substantial improvements in healthcare delivery; yet interventions of this kind are not implemented as widely as they could be (across trusts and healthcare priority issues). The diagram below provides an overview of ways in which behavioural insights could be applied to achieve this goal. These areas of focus have been selected either because they are areas where past behavioural interventions have delivered positive outcomes, or because interventions of this kind have been successful on similar issues elsewhere.