To mark World Health Day, we’re sharing the results of a trial helping people with diabetes in the Middle East and North Africa (MENA) region to reduce their blood sugar levels.
The MENA region presently has the highest regional prevalence of diabetes at 16.2%. Projected trends are troubling too: the diabetes rate is expected to grow by 86%, reaching 136 million by 2045. Without proper management, diabetes can lead to serious and chronic complications, including eye disease, cardiovascular diseases, and kidney failure.
In partnership with the national Health department, we ran an ambitious trial. It aimed to test whether supporting patients to make diet and lifestyle commitments (e.g., eating less rice) could lower blood sugar levels and BMI.
We didn’t find a significant effect on patients’ blood sugar. However, promising results for patients whose baseline blood sugar level was high offer interesting insights to build on for future work.
What we did
BIT conducted an evidence review and qualitative research in healthcare centres where the majority of people living with diabetes receive care. We found two broad issues that people with diabetes face:
- Lack of consistency in advice: there was no standard approach or consistent messaging to support patients to reduce their blood sugar levels.
- Healthier lifestyles can be hard in the moment: even when people know they should eat healthier and exercise more, the influence of social norms around eating and present bias – our tendency to overvalue immediate rewards, such as an unhealthy treat, over long-term benefits – made following through with healthy behaviours harder in reality.
To tackle these barriers, we ran a randomised controlled trial involving 624 patients in six PHCs to test two new interventions. We tested these against the existing information booklet that was provided to patients (control). The two treatments were:
- Treatment 1 – “Healthy commitments”: to address the lack of standardised advice and help overcome present bias, people completed a “My Diabetes Journey” card. They used this to set goals for reducing their blood sugar and choose actions they would take to achieve them (eg, reducing portion sizes). Patients also received feedback from their doctor.
- Treatment 2 – “Healthy commitments” and “care calls”: As well as the “My Diabetes Journey”, people received calls every two weeks from a nurse to monitor their progress and provide feedback to keep them on track.
Results and digging into the data
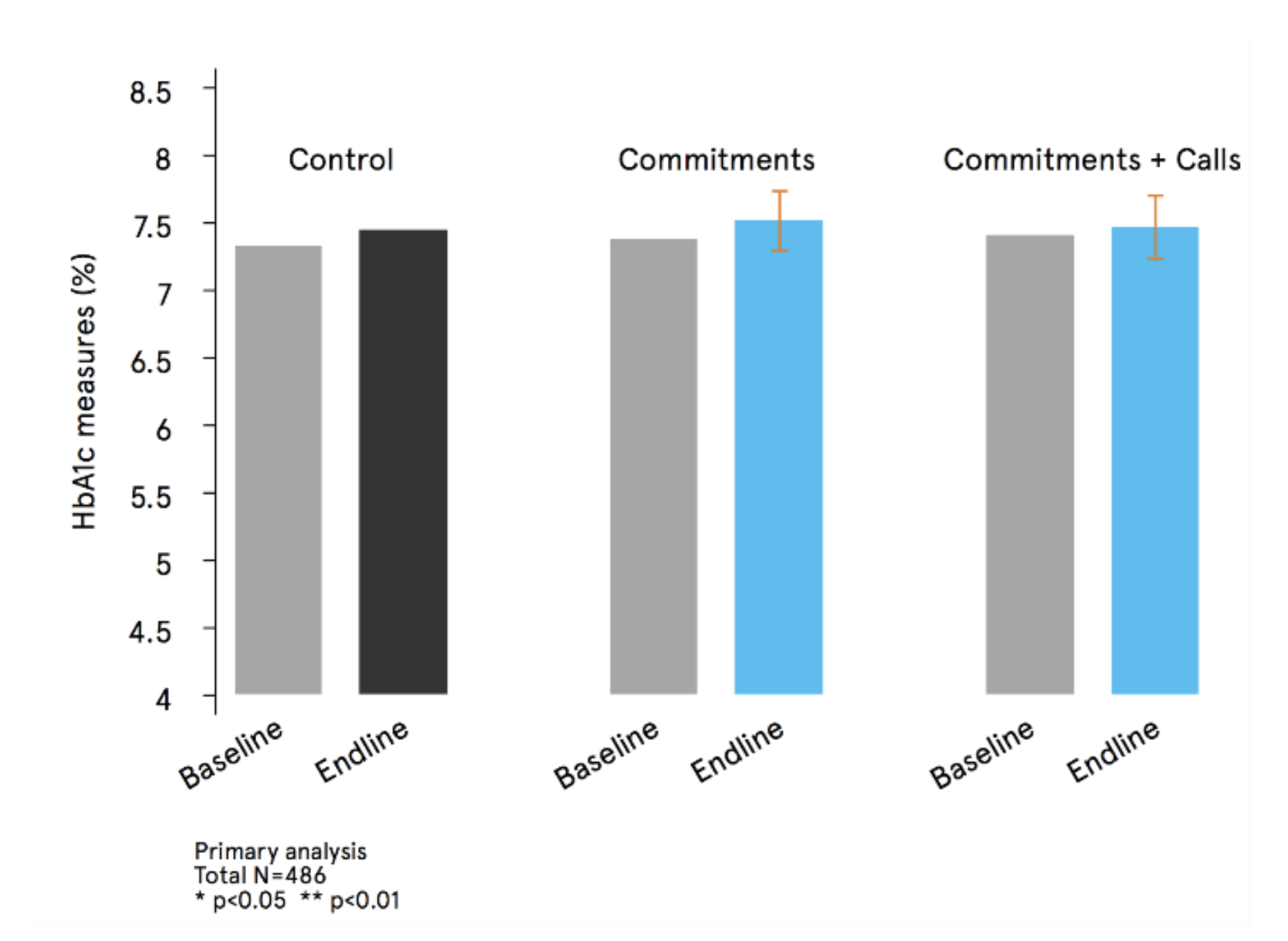
Neither the healthy commitments nor the addition of the monitoring calls had a statistically significant effect on people’s blood sugar levels compared to the existing leaflet.
 |
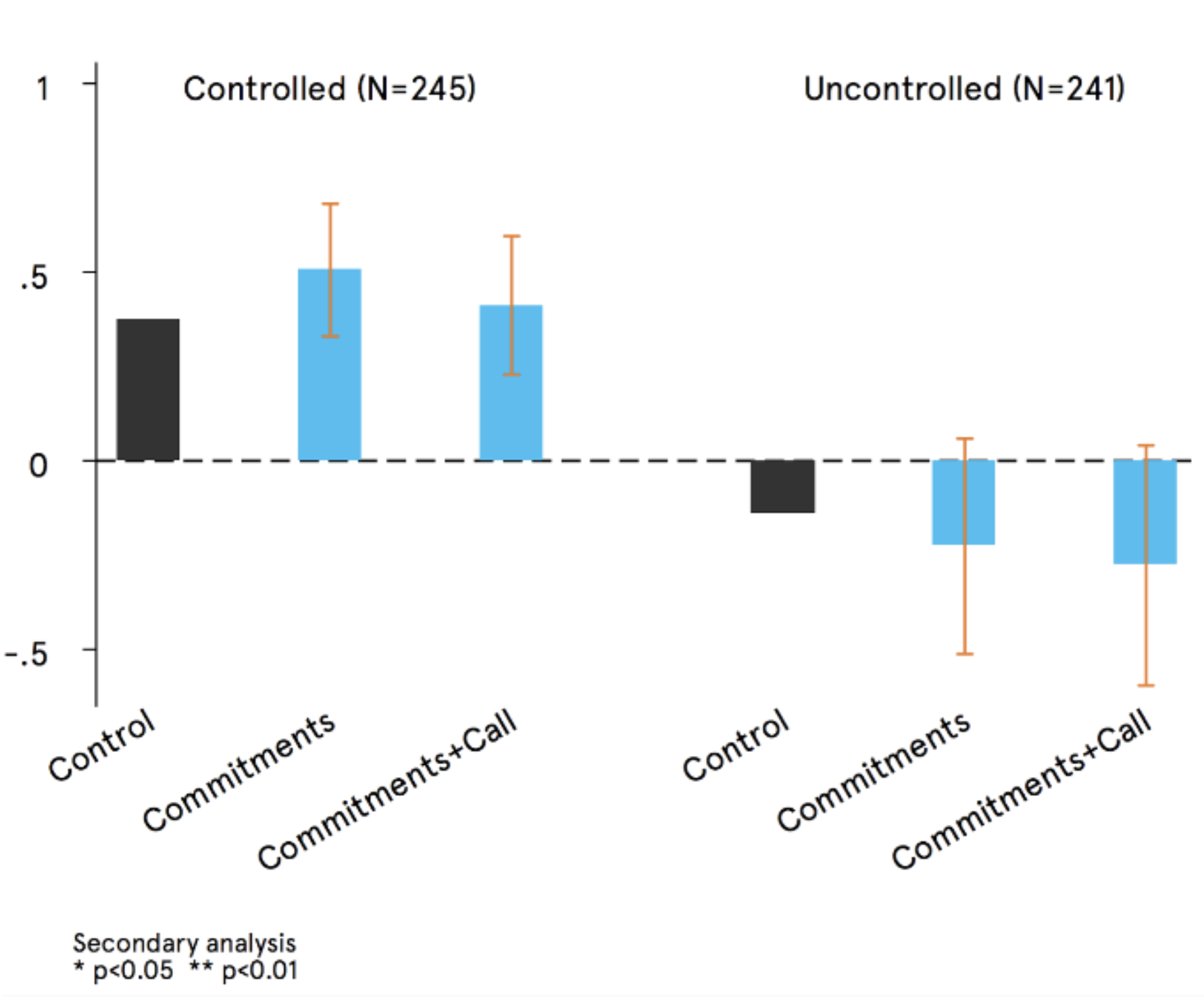 |
| Results for the two treatments compared with the control. | Sub-group analysis exploring the difference between people with “controlled” and “uncontrolled’ blood sugar levels |
However, further exploratory analysis revealed an intriguing finding. Patients with high “uncontrolled” blood sugar, as compared to those with low “controlled” blood sugar, showed positive signs of impact (although these were also not statistically significant).
While we had originally intended to impact a wider target population, this particular finding illustrates the importance of conducting subgroup analyses in research through digging deep into the data. By doing so, behavioural scientists can uncover what interventions are most effective for specific subgroups, and ultimately, tailor our strategies to maximise impact. In other words, it’s not just about what works – but what works and for whom.