Giving my evidence to the Covid Inquiry, I was sharply aware of the families sitting in the room. While the cameras are trained on you, the families sit with quiet dignity just off screen. Some sit with pictures of those who died. It is a powerful and important reminder of what the Inquiry is really about. They want answers. They want to know that lessons have been learnt. We all should.
The headlines have so far focused mainly on the drama and failings within No.10, and especially on the early months of the pandemic up until the first ‘lockdown’. But there is a danger that this focus crowds out a hard-headed analysis of the wider system failures that happened.
This matters not just because of covid. It matters because these same weaknesses lie at the heart of many aspects of the day-to-day underperformance of government. Where there should be evidence we get presumption, where there should be humility we too often get blind faith. So it was with the pandemic.
‘Behavioural fatigue’: decision-making at odds with behavioural science
When the former Prime Minister Boris Johnson gave his evidence to the Covid Inquiry, he put ‘behavioural fatigue’ back in the spotlight. Johnson stated: “I was told repeatedly, by both CSA and CMO, you know, you risked bounceback and behavioural fatigue and get more behavioural fatigue as a consequence of bounce-back”.
It’s not that it is a crazy notion. Some effortful behaviours – such as resisting desserts or persisting with taking medications when you are feeling better – are prone to decay (or ‘extinction’ as experimental psychologists call it). But sometimes it goes the other way: initially effortful behaviour can establish new habits and norms, such as cycling to work – or doing weird new things like wearing masks. ‘Behavioural fatigue’ isn’t an explanation – it’s a possibility contingent on many factors.
In the case of covid, there was strong evidence from multiple sources that most people would comply with tough measures and persist with them, especially if there was a clear justification. James Rubin et al provided an excellent early review, showing compliance with quarantine measures tended to be very high. Historic data from 1918-19, notably from US cities, similarly showed high compliance that only really started to crack in later lockdowns (indeed foreshadowing covid experience). Our own work and advice strongly reinforced this conclusion, not least because individual acts of compliance, involved whole populations mutually reinforcing each others behaviour (cf ‘declarative social norms’). In a relatively high social trust country like the UK, we were fairly confident that people would reinforce each others’ behaviour to ‘do the right thing’.
Reicher’s recent piece makes an additional important point, perhaps less discussed at the time. On many difficult tasks, people do become fatigued, but it doesn’t mean they give up. Going for a run is hard work, but it doesn’t mean you stop.
When Chris Whitty used the phrase ‘behavioural fatigue’ at that press conference, he also added that “part of the science on this is actually the behavioural science, and what that shows is probably common sense to everybody in this audience”. I think this is very telling. A big problem for behavioural science is that the very familiarity of the human subject gives us a false sense of confidence that ‘we know’ what drives human behaviour. In fact, behavioural science has thrown up all sorts of surprises. Indeed, it would be a pretty dull ‘science’ if it didn’t.
In the same way that we have learned to move beyond intuitions and ‘common sense’ in medicine, we need to do the same with respect to behaviour and policy.
The early missteps: flatten the curve
The former PM also highlighted the early expert advice in the UK – one might say presumption – was that once community transmission in the community took hold, covid would be unstoppable, a ‘wave’. In the face of this, the best that could be done was to ‘flatten the curve’, that is preventing further deaths as a result of the NHS being overwhelmed and an ‘overswinging’ epidemic. This was expressed as ‘contain-delay-mitigate’ when the Government published its strategy in early March.
In his evidence, Patrick Vallance notes:
‘I am not sure what an alternative strategy would have looked like at that time. The central problem for the UK was that it did not have the capacity to maintain the contain stage.’ [para 183]
We do know ‘what an alternative strategy would have looked like’ – and we had a pretty good idea at the time. It looked like South Korea: using mobile phone data to help track contacts; requiring and checking in-person that those identified did isolate; and supporting people to comply such as sending care packages with food and a thermometer. Or Germany, where they immediately recruited 20,000 extra contact tracers while the UK spoke about switching off tracing efforts.
Arguably even more damning than the UK’s early presumption of an unstoppable wave was the country’s deja vu moment in late summer 2020, once again facing the terrible choice of ‘lock-down’ or ‘let it rip’.
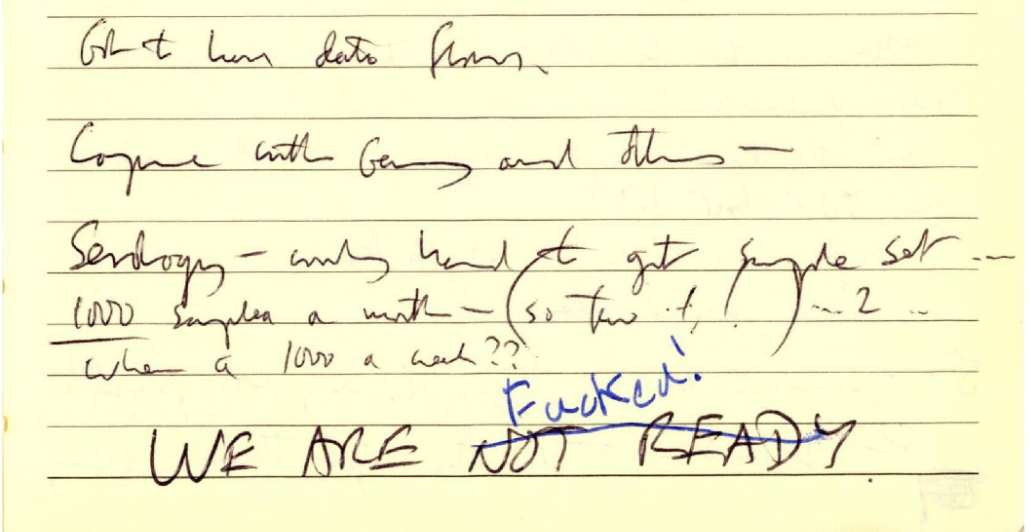
Viewed as a system, the UK covid performance looks very much like what James Reason has called a ‘swiss cheese’ failure: an alignment of multiple failures that leads to catastrophe. When I scribbled in my notepad ‘WE ARE NOT READY’ in SAGE on March 13th – just before the first lockdown – it wasn’t because of toxicity, indecision and bad language at No. 10. We had just heard a litany of tell-tale signs that the Government and our systems were not where they needed to be.
Image: my notepad from March 13th, 2020. No10 Data scientist Ben Warner, who was sitting to my right, leaned across and put a line through ‘NOT READY’ to replace it with the now-famous blunter words…
The UK had had the benefit of being one of the last countries to be hit by the full-force of covid. And yet there was confusion over core numbers, including the capacity of the NHS (the famous ‘red-line’). Our testing and tracing capacity was woefully inadequate and about to be switched off. And our modellers were telling us they were ‘100% sure’ while other countries pursued other directions.
The alternative to the ‘lock-down or let it rip’ dilemma was ‘sophisticated viral suppression’. This tactic required a blitz of practical, operational questions, many of them behavioural. How do we get people to wash their hands and open windows more often? How do we identify who is most likely to have the virus, to get tested, and to self-isolate? And later, how do we get people to come forward for vaccinations, and to remember that it doesn’t offer protection for the two weeks afterwards?
Most of these weren’t ‘high science’. SAGE and advisory bodies such as the Scientific Pandemic Insights Group on Behaviours (SPI-B) have since made clear that it wasn’t for them to answer such operational and delivery questions. But with covid, such operational capability was absolutely pivotal to the delivery of ‘sophisticated viral suppression’. Unfortunately, answering such ‘operational’ questions has never been a great strength of Whitehall – the classic ‘policy’ versus ‘delivery’ capability gap.
The weakness of our wider test, trace and isolate system illustrates the issue. From late February 2020, we failed to get 111 to ask for postcodes that would have enabled precise early geographic targeting, leaving modellers to rely on lagging and small sample data such as ICU numbers. The covid app that was promised for 3 weeks took 6 months. We did not pursue commercial alternatives to the app. We did not implement South Korean-style care packages. We did not implement financial support for self isolation until autumn 2020.
Learning the hard way
Cutting across all these examples is that we didn’t build systems – outside of drug trials and a few bits of comms – designed to experiment and improve. Rapid ‘test, learn, adapt’ approaches – the faster the better – upgrade your operational models and processes. In the case of covid, we didn’t need a system that was perfect. It ‘just’ needed to be good enough and getting better to clip that average re-infection rate down from 2.5 to 1. That would have been hard but not impossible.
Why does this matter? It is this same anti-experimental mindset – hubris over humility – that lies at the heart of underperformance in our public services and policy more generally. Our economic policies, at local and national level, plump for one tax subsidy or another, but almost never with systematic testing. Our criminal justice system is riven with rigid practices that have never been empirically tested. Our benefits and education systems do now have some testing, but far too many decisions are still based on untested presumptions.
We should not let our justified rage at Downing Street parties let the wider, systemic weaknesses of the UK government – and many others – off the hook. We need to build forms of government and delivery with humility, rapid experimentation and improvement into their core design. If covid teaches us this core lesson, it will save and transform many lives in the years to come.