GDPR has made us all more aware of how our personal data is shared and collected. But how much do we understand the data sharing choices presented to us? It’s a question especially relevant in the context of the UK National Health Service, which collects and analyses a range of personal information.
What is confidential patient information?
Confidential patient information is data collected about you when you visit NHS services. It includes details about your health, care or treatment – information you would expect to be kept private. The NHS collects this data for three main reasons: to help manage people’s individual care, to help research new treatments, and to help plan health and care services. But do people really grasp the difference between “research” and “planning”?
In layman’s terms, “research” might mean finding new cures for diseases, and “planning” probably covers use of resources. But through our recent work with the National Data Opt-out Programme (NDOP), we learned it can be hard for people to distinguish the difference in the complicated world of confidential patient data – which in turn can impact their data use decisions.
In 2016, the National Data Guardian recommended that people should be able to easily opt out of their confidential patient data being used for research and planning. Earlier this year, NDOP implemented this recommendation by launching an online tool and a supporting call centre service that allows people to state their data sharing preference. This single decision is then applied across the entire health and care system, though people can change their preference at any time.
How BIT and NDOP tested people’s understanding of “research” and “planning”
Before launching this website, NDOP wanted to know whether they should give people:
- a simple choice of sharing their data (or not) for research and planning
- the choice to share their data for research only, planning only, both planning and research, or neither.
The second option might seem superior, since it gives people more freedom of choice. However, a key question was whether members of the public actually understood what the NDOP meant when it talked about using data for “research” and “planning”. Importantly, they needed to understand what these words meant in terms of how they are used by the NHS to classify different uses of confidential patient information, not what they mean in layman’s language. If they did understand the difference, then it would make sense to offer them the choice of selectively opting out of research only or planning only. If most people found it hard to tell the difference, it might then make more sense to offer them a simpler choice of opting out of “research and planning” as a combined category.
In 2017, BIT and NDOP ran two online experiments to provide empirical guidance on this issue. These experiments were run on BIT’s in-house experimental platform Predictiv and used large, England-representative samples. In the experiments, we showed people hypothetical case studies describing uses of patient data, such as the case outlined below:
“GP clinics regularly measure the height and weight of their patients. They share this information with NHS Digital, which analyses the data. A local team, led by GPs, use this data to look at their local population. They see that obesity rates in specific postcode area have risen from 7% to 13% in the last five years. They recommend opening a new clinic in the area to provide dietary advice and weight-loss programmes.”
After seeing a case study, people were asked what people’s data being was used for in the example.
- In Experiment 1, people were asked whether they thought the data was being used for “research and planning”, “research only”, “planning only”, or “individual care”.
- In Experiment 2, they were asked whether the data was being used for “individual care” or “research and/or planning”.
We designed the experiments this way because we thought that while people could probably tell the difference between the use of data for their individual care, rather than for research and planning, we suspected they would find it much harder to tell the difference between data being used for research or planning only. In fact, we often had trouble understanding the difference ourselves.
Figure 1 shows the results. In Experiment 1, only 1 in 5 (22%) said “Planning only”, the technically correct answer. In Experiment 2, which gave people the easier task of only identifying whether the data was being used for “individual care” or “research and/or planning”, 84% of people correctly said the latter.
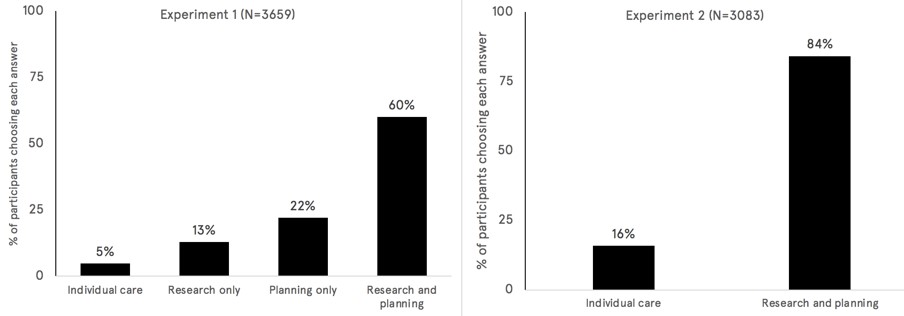
We tested several other case studies with similar results – people had a good intuitive sense for when data was being used for “research and planning” as a combined category, but found it very challenging to tell the difference between uses of data for research only vs planning only.
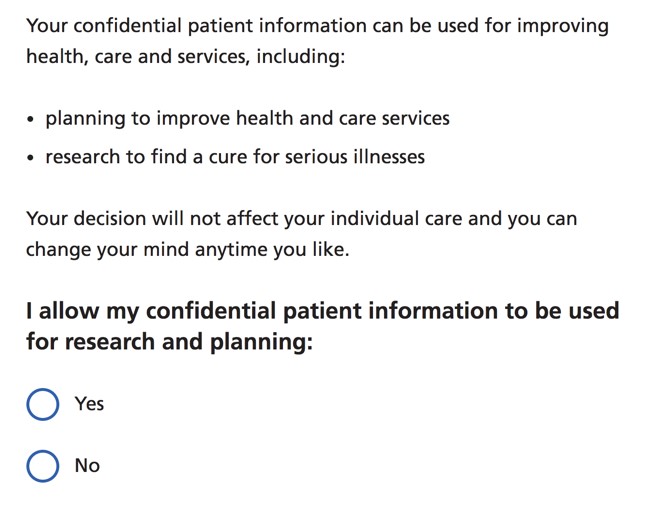
Partly as a result of this research, the NDOP website has now been designed to offer people the simple choice of sharing their data (or not) for “research and planning” as a combined category, as shown in Figure 2.
This is a good example of how careful empirical work can inform the design of government policy. The online testing enabled us to quickly test a realistic version of the website on a nationally-representative sample of thousands of adults in England.
We think this approach could be used to inform the design of many other government policies, not just those relating to personal data. People in government will always need to make decisions about how to present options to the public – these findings demonstrate that behavioural insights can improve the extent to which the choices that government offer are evidence based.